Retinal detachment is a serious condition that requires timely diagnosis and appropriate treatment to prevent vision loss. Understanding the different types of retinal detachment, the diagnostic techniques available, and the treatment options can help patients make informed decisions about their care. In this article, we will explore the various aspects of retinal detachment and discuss the effective treatments available.
Understanding Retinal Detachment
The Anatomy of the Eye
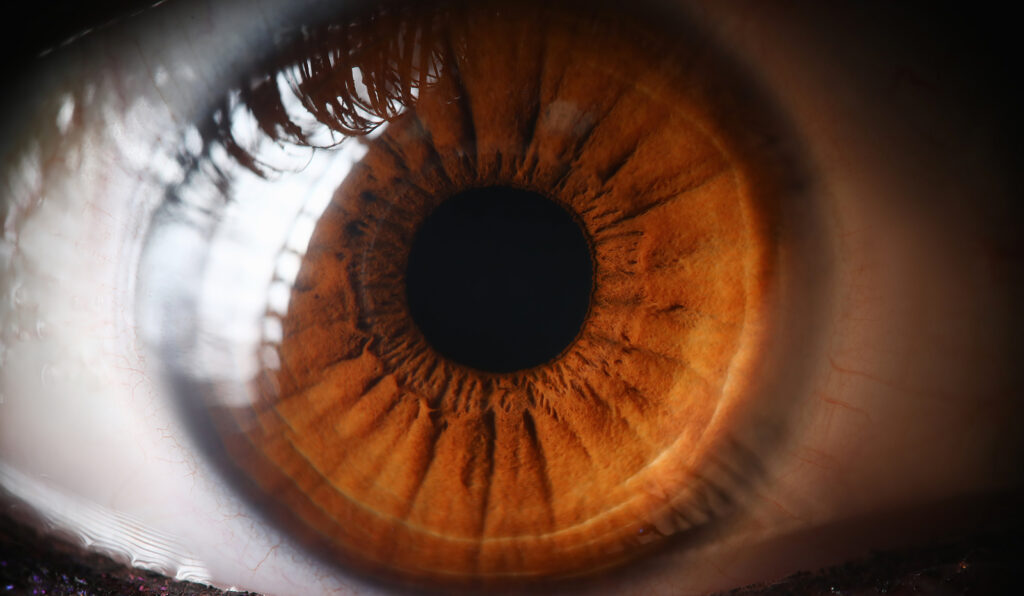
The eye is a marvel of biological engineering, comprising intricate components that harmoniously work together to enable the sense of vision. Among these components, the retina stands out as a vital player in the visual process. Positioned at the posterior part of the eye, the retina acts as a light-sensitive layer that captures incoming light rays and converts them into neural signals, which are then relayed to the brain for interpretation. This complex cascade of events is fundamental to our ability to perceive the world around us with clarity and detail.
Moreover, the retina is not a uniform structure but consists of distinct layers, each with specialized functions contributing to visual acuity. These layers work in concert to ensure that the visual information received by the eye is accurately processed and transmitted to the brain for meaningful interpretation. Any disruption to this intricate system, such as retinal detachment treatments, can have profound implications for vision and overall ocular health.
Causes and Symptoms of Retinal Detachment
Retinal detachment can arise from a myriad of factors, ranging from sudden trauma to the eye, degenerative changes associated with aging, to underlying ocular conditions like myopia or diabetic retinopathy. The onset of retinal detachment is often heralded by a cluster of distinct symptoms that should not be ignored. These symptoms may manifest as the abrupt onset of floaters—small, dark spots drifting in the visual field, flashes of light akin to lightning bolts, and the perception of a shadow or curtain descending over the field of vision. Recognizing these warning signs and seeking immediate medical intervention is paramount in mitigating the risk of irreversible vision loss.
Furthermore, the treatment for retinal detachment typically involves surgical intervention aimed at reattaching the detached retina to its original position and restoring visual function. Various surgical techniques, such as scleral buckling or vitrectomy, may be employed based on the severity and extent of the detachment. Timely diagnosis and intervention play a pivotal role in the prognosis of retinal detachment, underscoring the importance of regular eye examinations and proactive eye care to safeguard ocular health.
Types of Retinal Detachment
Rhegmatogenous Retinal Detachment
Rhegmatogenous retinal detachment is the most common type and occurs when a tear or hole develops in the retina, allowing fluid to accumulate between the retina and its underlying tissue. This can lead to the detachment of the retina, impairing vision.
Rhegmatogenous retinal detachment often occurs spontaneously, but it can also be associated with trauma to the eye or previous eye surgeries. The accumulation of fluid behind the retina causes it to separate from the underlying layers, leading to symptoms such as sudden flashes of light, floaters in the field of vision, and a curtain-like shadow over the visual field. If left untreated, this type of detachment can result in permanent vision loss. To read more about vision loss click here.
Tractional Retinal Detachment
Tractional retinal detachment occurs when scar tissue or abnormal blood vessels exert traction on the retina, pulling it away from its normal position. Conditions such as diabetic retinopathy can contribute to this type of detachment.
In diabetic retinopathy, the growth of abnormal blood vessels can cause fibrous scar tissue to develop on the surface of the retina. As this scar tissue contracts, it can distort the shape of the retina and pull it away from the underlying tissues, leading to tractional retinal detachment. Patients with this condition may experience gradual blurring of vision, distortion of shapes, and difficulty seeing in low light conditions.
Exudative Retinal Detachment
Exudative retinal detachment occurs when fluid leaks into the area between the retina and its supportive tissues, usually due to a disorder affecting the blood vessels. This type of detachment is less common but can still cause vision problems.
Conditions such as age-related macular degeneration or inflammatory disorders can lead to exudative retinal detachment. In these cases, abnormal blood vessels or inflammation can cause fluid to accumulate under the retina, leading to a separation of the layers. Patients with exudative retinal detachment may experience a sudden decrease in central vision, distortion of straight lines, and difficulty recognizing faces.
Diagnosis of Retinal Detachment
Clinical Examination
Diagnosing retinal detachment typically involves a comprehensive eye examination. Your ophthalmologist will evaluate your symptoms, conduct a visual acuity test, and examine the back of your eye using specialized instruments to assess the condition of the retina.
During the clinical examination, your ophthalmologist will also perform a detailed assessment of your medical history to identify any underlying conditions or risk factors that may contribute to retinal detachment. This holistic approach helps in determining the most appropriate treatment plan tailored to your individual needs.
Imaging Techniques
In addition to a clinical examination, your ophthalmologist may utilize imaging techniques such as optical coherence tomography (OCT) or ultrasound to gather more detailed information about the retina and determine the extent and location of the detachment.
Optical coherence tomography (OCT) is a non-invasive imaging test that uses light waves to capture high-resolution cross-sectional images of the retina. This technology allows for the visualization of the different layers of the retina, helping the ophthalmologist to precisely locate any areas of detachment and monitor the response to treatment over time.
Treatment Options for Retinal Detachment
Surgical Procedures
Surgery is the most common method for treating retinal detachment. Depending on the type and severity of the detachment, different surgical techniques may be employed. These procedures aim to reposition the retina and seal any tears or holes to prevent further detachment.
One common surgical procedure for retinal detachment is scleral buckling. During this procedure, a silicone band is placed around the eye to gently push the wall of the eye against the detached retina, helping it to reattach. Another surgical option is vitrectomy, where the vitreous gel inside the eye is removed and replaced with a gas bubble to push the retina back into place. Learn more about vitrectomy at https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=135&contentid=385
Laser Therapy
Laser therapy, also known as photocoagulation, uses focused beams of light to create small burns around the retinal break or tear. This process helps to create scar tissue that seals the retina and prevents further detachment.
It is important to note that laser therapy is often used for small retinal tears or holes that have not yet progressed to a full detachment. The procedure is typically quick and can be done in an outpatient setting, with minimal discomfort for the patient. However, laser therapy may not be suitable for all types of retinal detachments, and your ophthalmologist will determine the most appropriate treatment plan for your specific condition.
Cryotherapy
Cryotherapy involves the use of extreme cold to freeze the area around the retinal tear or detachment. Freezing the tissue creates scars, which act as barriers to prevent further separation of the retina.
While cryotherapy can be effective in treating retinal detachments, it is often used in combination with other surgical techniques for optimal results. The procedure is performed under local or general anesthesia, and the cold temperature is carefully controlled to ensure the safety of the surrounding eye structures. Cryotherapy may cause some temporary discomfort or redness in the eye, but these symptoms typically resolve as the eye heals.

Post-Treatment Care and Recovery
Follow-up Visits and Monitoring
Following retinal detachment treatment, close monitoring is essential to ensure proper healing and detect any recurrent or new changes. Regular follow-up visits with your ophthalmologist will allow them to evaluate your progress and make any necessary adjustments to your treatment plan.
During these follow-up visits, your ophthalmologist will conduct thorough examinations of your eyes, which may include visual acuity tests, intraocular pressure measurements, and detailed retinal evaluations. These evaluations help in assessing the success of the treatment and identifying any signs of complications early on. Your ophthalmologist will also discuss any symptoms or concerns you may have, providing you with the opportunity to address them promptly.
Lifestyle Adjustments for Recovery
During the recovery phase, it is important to take certain precautions to optimize healing. Your ophthalmologist may recommend avoiding activities that put strain on the eyes, such as heavy lifting or vigorous exercise. Additionally, proper nutrition and maintaining a healthy lifestyle can facilitate recovery.
Engaging in relaxation techniques, such as deep breathing exercises or meditation, can also be beneficial during the recovery period. These practices not only help reduce stress and anxiety but also promote overall well-being, which is essential for the healing process. Adequate rest and sleep are equally important, as they allow your body, including your eyes, to recuperate and regenerate effectively.
Read more




