Sleep is an essential part of our daily lives. It plays a crucial role in maintaining our overall health and well-being. The quality and quantity of sleep we get can have a significant impact on our physical and mental health. Understanding sleep patterns can provide valuable insights into our overall health and help identify potential issues that may need attention. In this article, we will delve into the importance of sleep, the science behind sleep, and why sleep patterns matter. We will also explore the process of analyzing sleep patterns and take a closer look at the specific sleep patterns observed in Canberra, the capital territory of Australia. Additionally, we will examine the relationship between sleep and health and discuss strategies for improving sleep patterns.
Understanding the Importance of Sleep
Sleep is not just a period of rest and downtime for our bodies; it is a complex and dynamic process that plays a vital role in our overall well-being. During sleep, our bodies undergo various physiological and cognitive processes that are essential for physical and mental health. A lack of quality sleep can lead to a range of health issues, including fatigue, decreased cognitive function, weakened immune system, and an increased risk of chronic conditions such as obesity, diabetes, and cardiovascular disease.
Canberra, the capital territory of Australia, is home to a diverse population with unique sleep patterns. Various factors influence sleep patterns in Canberra, including lifestyle, work demands, environmental factors, and individual differences. Therefore it is necessory to conduct sleep study canberra.
Getting adequate sleep is important for maintaining optimal brain function, supporting learning and memory processes, and promoting emotional and mental well-being. It also plays a crucial role in regulating the body’s hormone levels, including those that control appetite, metabolism, and stress responses.
The Science Behind Sleep
While the exact mechanisms of sleep are not yet fully understood, researchers have made significant progress in unraveling the mysteries of sleep. Sleep is a complex interplay of various physiological processes, including changes in brain activity, body temperature, heart rate, and hormone levels.
There are two main types of sleep: rapid eye movement (REM) sleep and non-rapid eye movement (NREM) sleep. REM sleep is characterized by rapid eye movements and vivid dreaming, while NREM sleep is further divided into three stages – N1, N2, and N3, with N3 being the deepest stage of sleep.
Throughout the night, our sleep cycles oscillate between REM and NREM sleep in a pattern that repeats approximately every 90 minutes. These cycles play a crucial role in consolidating memories, regulating emotions, and restoring our bodies.

Why Sleep Patterns Matter
Sleep patterns, including the duration, timing, and quality of sleep, can provide valuable insights into our overall health and well-being. They are influenced by a range of factors, including lifestyle, environmental factors, and individual differences.
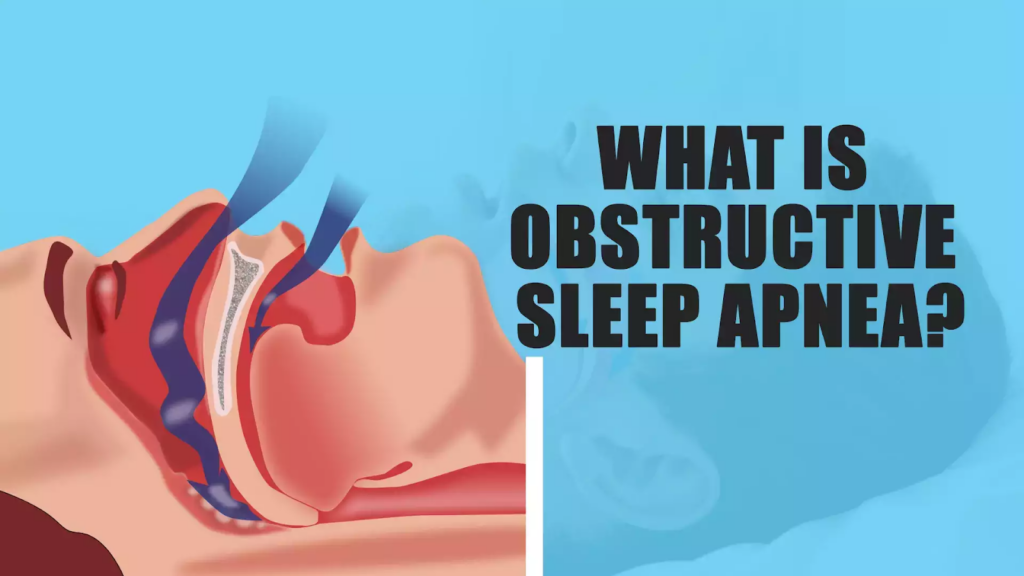
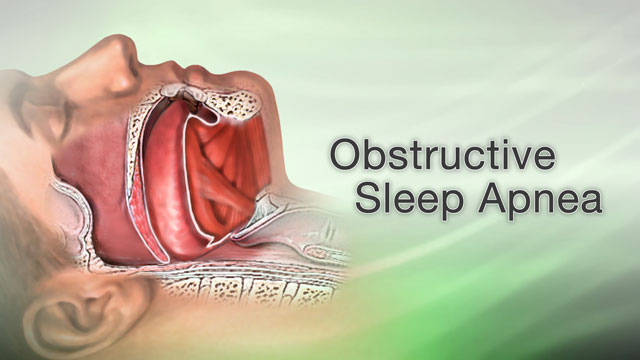
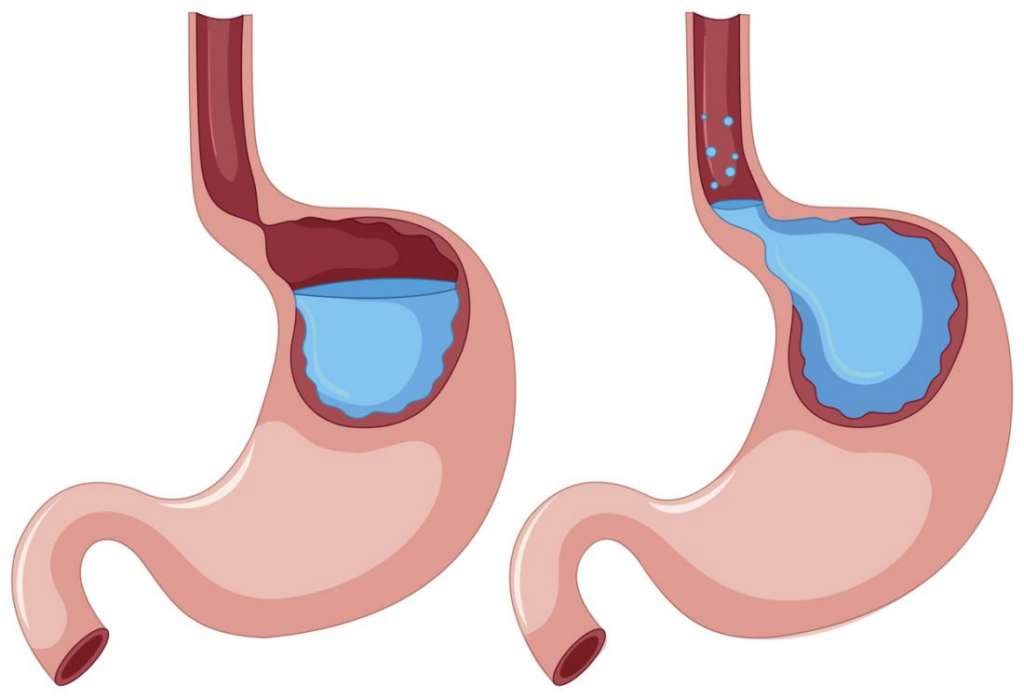
Disruptions in sleep patterns, such as insomnia, sleep apnea, or shift work, can have a negative impact on our physical and mental health. They can lead to daytime sleepiness, impaired cognitive function, mood disturbances, and an increased risk of accidents or errors.
By analyzing sleep patterns, researchers can identify potential sleep disorders or underlying health issues that may need intervention. They can also provide recommendations for improving sleep quality and developing strategies for better sleep hygiene. Learn more about better sleep hygiene visit at https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/sleep-hygiene.
The Role of Dreams in Sleep
One fascinating aspect of sleep is the role that dreams play during the REM stage. Dreams are a product of our brain’s activity during sleep and can range from mundane to fantastical. They often reflect our emotions, experiences, and subconscious thoughts.
While the exact purpose of dreaming is still debated among scientists, some theories suggest that dreams may help with memory consolidation, emotional processing, and problem-solving. They may also serve as a way for our brain to process and make sense of the information we encounter during wakefulness.
Research has shown that individuals who are deprived of REM sleep, and thus dream sleep, experience negative effects on their mood, cognitive function, and overall well-being. This highlights the importance of allowing our brains to engage in this unique and mysterious aspect of sleep.
The Process of Analysing Sleep Patterns
Analyzing sleep patterns involves the use of various tools and techniques to gather data and interpret the results. These tools can range from wearable devices that track sleep duration and quality to more advanced methods such as polysomnography, which measures brain wave activity, eye movements, and muscle tone during sleep.
The collected data is then analyzed to identify patterns, such as sleep efficiency, sleep latency, and the distribution of different sleep stages throughout the night. Interpretation of these patterns can provide valuable insights into sleep quality, potential sleep disorders, and the overall health of an individual.
Tools and Techniques for Sleep Analysis
There are several tools and techniques used in sleep analysis, depending on the specific needs and objectives of the study. These may include:
- Actigraphy: This method uses a wearable device, usually worn on the wrist, to measure and record movement patterns. It provides information on sleep duration, restlessness, and sleep efficiency.
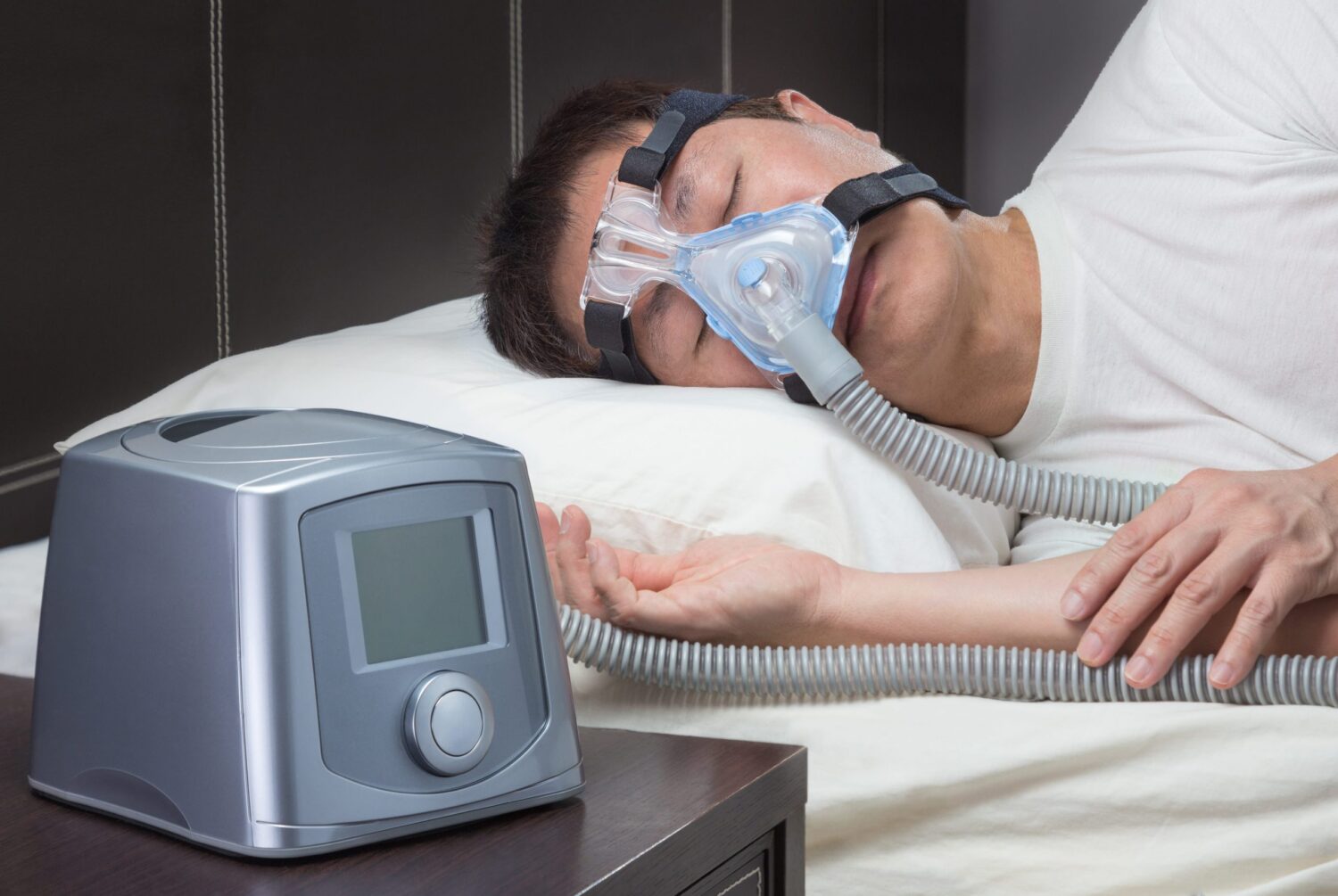
- Polysomnography: This comprehensive sleep test involves monitoring brain activity, eye movements, heart rate, muscle tone, and breathing patterns during sleep. It is often used to diagnose sleep disorders such as sleep apnea or narcolepsy.
- Sleep diaries: These self-reported logs are used to track sleep-related variables, including bedtime routine, sleep duration, and perceived sleep quality. They provide subjective information and can be used alongside other objective measures.
Actigraphy is particularly useful for long-term sleep monitoring, as it allows individuals to track their sleep patterns in their natural environment. Polysomnography, on the other hand, provides a more comprehensive assessment of sleep physiology and is often conducted in a sleep laboratory under controlled conditions. Learn more about Bulk Bill Sleep Study: Affordable Sleep Assessments for Everyone visit at https://healthonlinezine.info/bulk-bill-sleep-study-affordable-sleep-assessments-for-everyone/.
In addition to these tools, researchers and sleep professionals also utilize other techniques such as electroencephalography (EEG), which measures electrical activity in the brain, and actimetry, which assesses physical activity levels during sleep. These additional measures help to further refine the analysis and provide a more detailed understanding of an individual’s sleep patterns.
Interpreting Sleep Data
Interpreting sleep data requires expertise and a thorough understanding of sleep physiology and the factors that influence sleep patterns. Sleep professionals use various parameters to analyze sleep data, including sleep efficiency, total sleep time, wake after sleep onset, and the distribution of different sleep stages throughout the night.
Combining objective sleep data with subjective reports, such as sleep diaries or patient questionnaires, helps in obtaining a comprehensive understanding of an individual’s sleep patterns and identifying potential sleep disorders or areas for improvement.
Furthermore, advancements in technology have led to the development of sophisticated algorithms that can analyze large amounts of sleep data and provide detailed insights. These algorithms can detect subtle changes in sleep patterns over time and help researchers identify trends or anomalies that may be indicative of specific sleep disorders or underlying health conditions.
Overall, the process of analyzing sleep patterns is a multidimensional approach that combines various tools, techniques, and expertise to gain a comprehensive understanding of an individual’s sleep health. By unraveling the mysteries of sleep, researchers and sleep professionals can contribute to the development of effective interventions and treatments for sleep disorders, ultimately improving the quality of life for individuals worldwide.

Sleep Patterns in Canberra: An Overview
Factors Influencing Sleep Patterns in Canberra
The fast-paced lifestyle of a city like Canberra can contribute to irregular sleep patterns. Work-related stress, long commuting hours, and shift work can disrupt the natural sleep-wake cycle.
Environmental factors, such as noise pollution or extreme temperatures, can also affect sleep quality and duration. Additionally, individual factors, such as age, health conditions, and personal habits, can further influence sleep patterns in Canberra. Learn more about noise pollution click here.
The Impact of Lifestyle on Sleep Patterns
Lifestyle choices play a significant role in shaping sleep patterns. Engaging in regular physical activity, maintaining a balanced diet, and managing stress can positively impact sleep quality. On the other hand, unhealthy habits, such as excessive alcohol consumption, smoking, or irregular sleep schedules, can disrupt sleep patterns.
Creating a sleep-friendly environment, both physically and mentally, can also contribute to better sleep in Canberra. This includes optimizing bedroom conditions, such as temperature, light exposure, and noise level, as well as establishing a consistent bedtime routine to signal the body’s natural sleep-wake cycle.
The Relationship Between Sleep and Health
Sleep has a profound impact on our physical and mental health. It is not just a time of rest; it is a critical period for bodily rejuvenation and repair.
Sleep and Physical Health
Quality sleep is essential for maintaining optimal physical health. During sleep, the body repairs tissues, restores energy levels, and regulates various physiological processes. A lack of sleep can disrupt these processes and contribute to a range of health issues, including weakened immune function, increased inflammation, and an elevated risk of chronic conditions such as obesity, diabetes, and cardiovascular disease.
On the other hand, prioritizing sleep and ensuring adequate rest can enhance immune function, support healthy weight management, and promote overall physical well-being.
Sleep and Mental Health
Sleep plays a critical role in maintaining optimal mental health. It supports cognitive processes such as memory consolidation, learning, and problem-solving. A lack of quality sleep can impair cognitive function, contribute to mood disturbances, and increase the risk of mental health disorders such as depression and anxiety.
Conversely, prioritizing sleep and practicing good sleep hygiene can improve mental clarity, emotional well-being, and overall psychological resilience.
Improving Sleep Patterns: Tips and Strategies
If you are looking to improve your sleep patterns, there are several strategies you can implement to promote better sleep quality and duration.
Creating a Sleep-Friendly Environment
Optimizing your sleep environment can have a significant impact on sleep quality. Ensure your bedroom is dark, quiet, and at a comfortable temperature. Consider using blackout curtains, earplugs, or white noise machines to minimize disruptions.
Avoid using electronic devices, such as smartphones or tablets, before bedtime, as the blue light emitted by these devices can disrupt your natural sleep-wake cycle. Instead, engage in relaxing activities, such as reading a book or taking a warm bath, to promote relaxation and prepare your body for sleep.
The Role of Diet and Exercise in Sleep Quality
Regular physical activity can improve sleep quality and duration. Engaging in moderate-intensity exercise, such as walking or jogging, can help regulate sleep patterns and reduce the time it takes to fall asleep.
Avoid consuming stimulating substances close to bedtime, such as caffeine or nicotine. Instead, opt for sleep-promoting foods, such as turkey, almonds, or chamomile tea, which contain compounds that support relaxation and sleep.
Establishing a consistent sleep schedule, including a regular bedtime and wake-up time, can also help regulate your body’s internal clock and improve sleep quality over time.In conclusion, analyzing sleep patterns can provide valuable insights into our overall health and well-being. By understanding the importance of sleep and the science behind it, we can take steps to improve our sleep quality. In Canberra, factors such as lifestyle and environment influence sleep patterns, highlighting the need for strategies to optimize sleep in the city. Prioritizing sleep and adopting healthy habits can have a profound impact on both physical and mental health. By creating a sleep-friendly environment and incorporating regular exercise and a balanced diet, we can enhance our sleep patterns and embrace the benefits of a good night’s sleep.