Laser eye surgery has become a popular option for individuals seeking to correct their vision problems without relying on glasses or contact lenses. But not everyone is an ideal candidate for this type of procedure. Understanding who qualifies for laser eye surgery is essential for anyone considering the procedure. This article breaks down the complexities surrounding laser eye surgery and outlines the key factors that determine a good candidate.
Understanding Laser Eye Surgery
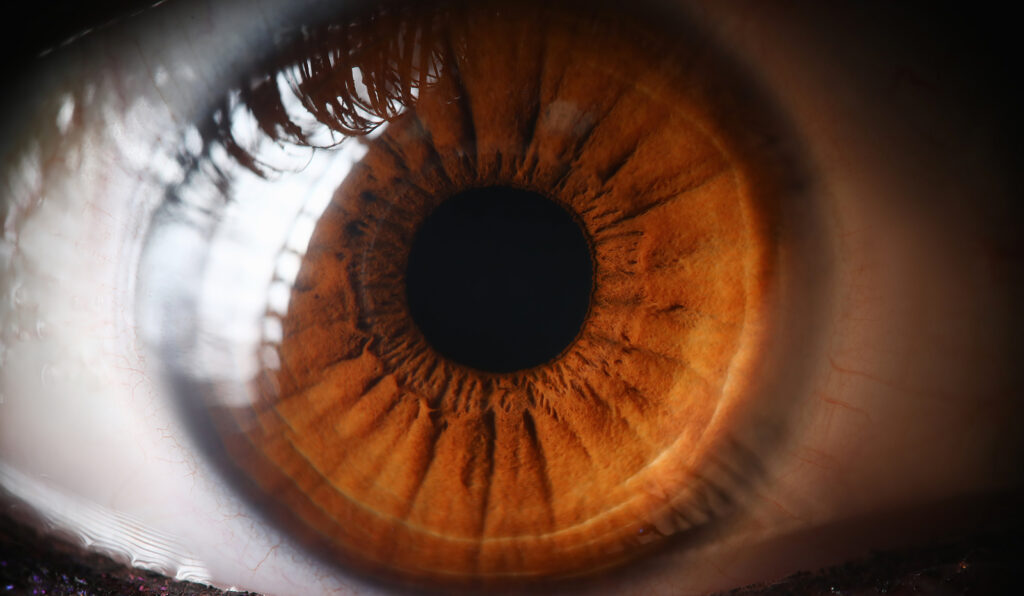
Laser eye surgery refers to various procedures aimed at improving vision by reshaping the cornea, which is the outer layer of the eye. This reshaping can correct common refractive errors such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. As technology advances, laser techniques have evolved, making surgeries more effective and safer than ever before.
In conclusion, while best laser eye surgery has the potential to transform lives, not every individual is a suitable candidate. Understanding the different types of laser eye surgery, evaluating personal health factors, and openly discussing concerns with a medical professional are essential steps toward making an informed decision. For those who qualify, the rewards often outweigh the risks, leading to enhanced vision and quality of life.
The Science Behind Laser Eye Surgery
The underlying principle of laser eye surgery is based on the use of focused light beams to reshape the cornea. The intuition behind this method lies in the fact that light must enter the eye in a certain manner to focus correctly on the retina. When the cornea is unevenly shaped, light cannot focus properly, leading to blurry vision. By using excimer lasers, surgeons can precisely remove microscopic amounts of tissue to create a more uniform corneal surface.
Modern lasers are guided by detailed measurements taken of the eye’s unique characteristics. This technology allows for personalized treatment plans, significantly enhancing the chances of a successful outcome. The recovery time for laser eye surgeries is generally quick, with many patients experiencing improved vision within hours or days after the procedure. Additionally, advancements in laser technology have led to the development of wavefront-guided LASIK, which takes into account higher-order aberrations, providing even more precise corrections tailored to the individual’s visual needs.

Different Types of Laser Eye Surgery
There are primarily three types of laser eye surgeries that are well-recognized and commonly performed:
- LASIK: The most popular form of laser eye surgery, LASIK involves creating a thin flap in the cornea, which is lifted to expose the underlying tissue. The laser then reshapes the cornea before the flap is replaced.
- PRK (Photorefractive Keratectomy): In PRK, the outer layer of the cornea is removed entirely before the underlying tissue is reshaped. The outer layer grows back over time, which may result in a longer recovery period compared to LASIK.
- LASEK (Laser Epithelial Keratomileusis): Similar to PRK, LASEK involves loosening the surface layer of the cornea with alcohol before reshaping the underlying tissue. This approach may offer benefits for individuals with thinner corneas.
Each type of surgery has its specific applications and benefits, making it essential for candidates to consult with an eye care professional to determine which is most suitable for their condition. Moreover, the choice of procedure can also depend on factors such as the patient’s age, lifestyle, and the severity of their refractive error. For instance, athletes or those with active lifestyles may prefer LASIK due to its quicker recovery time, while individuals with dry eyes might find PRK to be a more suitable option.
It’s also worth noting that laser eye surgery is not just limited to correcting refractive errors; it can also be used to treat other eye conditions such as keratoconus, a progressive thinning of the cornea. In such cases, specialized techniques like corneal cross-linking may be employed in conjunction with laser procedures to stabilize the cornea and improve vision. As research continues to advance in this field, the potential applications of laser technology in ophthalmology are expanding, promising even more innovative solutions for vision correction in the future. Read more about conjunction on https://writingcenter.uagc.edu/conjunctions
Determining a Good Candidate
While laser eye surgery has helped millions achieve clearer vision, not everyone is suitable for these procedures. There are several factors that potential candidates need to take into account, including their age, overall health, and specific vision issues.
Age and Laser Eye Surgery
Age is one of the first considerations in determining candidacy for laser eye surgery. Ideally, candidates should be at least 18 years old, as patients’ eyes must be fully developed before undergoing such procedures. Furthermore, vision should have stabilized for at least a year, meaning that significant prescription changes should have ceased.
Interestingly, while younger individuals are often more adaptable and tend to heal faster, older candidates may have age-related vision issues, such as presbyopia. This condition affects the ability to focus on close objects and may require additional types of vision correction even after surgery. Additionally, older patients may also experience other age-related eye conditions, such as macular degeneration, which can complicate the surgical process and outcomes.
Health Conditions and Laser Eye Surgery
Various health conditions can affect a person’s suitability for laser eye surgery. Candidates should ideally be in good overall health without any serious underlying conditions that could impede healing, such as autoimmune diseases or uncontrolled diabetes.
Additionally, eye conditions such as glaucoma, cataracts, and severe dry eye can disqualify candidates from undergoing laser eye procedures. Candidates should provide their eye care professional with a complete medical history to ascertain the risks associated with surgery. Furthermore, certain medications can also impact healing and recovery, so it’s crucial for candidates to discuss their current prescriptions with their eye care specialist. This comprehensive evaluation ensures that the benefits of laser eye surgery outweigh the potential risks, leading to the best possible outcomes for the patient.
Moreover, lifestyle factors such as smoking and excessive sun exposure can also play a significant role in determining candidacy. Smoking has been linked to a higher risk of complications during and after surgery, while prolonged sun exposure can exacerbate certain eye conditions. Candidates are often encouraged to adopt healthier habits and protect their eyes from UV rays prior to undergoing any surgical procedures, as these changes can enhance overall eye health and improve surgical results.
Benefits of Laser Eye Surgery
For those who do qualify, the benefits of laser eye surgery can be significant and life-changing. Many patients experience dramatic improvements in their vision, leading to a newfound sense of freedom from corrective lenses.
Long-Term Vision Improvement
One of the most compelling reasons to consider laser eye surgery is the potential for long-term vision improvement. Research has shown high success rates, with many patients achieving 20/25 vision or better after the procedure. This level of correction is adequate for many daily activities, including driving.
Moreover, as advancements in laser technology continue, outcomes become even more reliable, making the spectrum of vision correction broader. Patients moving away from glasses or contacts often report increased confidence and an improvement in their overall quality of life.
Lifestyle Changes After Surgery
Another significant benefit of laser eye surgery is the lifestyle changes that it promotes. Patients no longer need to worry about the inconvenience of maintaining glasses or dealing with the discomfort of contact lenses.
- Participating in sports and outdoor activities becomes easier without the worry of losing or damaging prescription eyewear.
- Traveling can be more spontaneous as patients can avoid packing lens solutions and ensuring they have spare glasses on hand.
- Daily routines, such as swimming or showering, can become hassle-free, allowing individuals to enjoy experiences that were previously challenging.
Risks and Considerations
While the benefits are appealing, potential candidates must also consider the risks associated with laser eye surgery. Like any medical procedure, laser eye surgery does carry certain risks that must be weighed against the benefits.
Potential Side Effects of Laser Eye Surgery
Even though most patients achieve good results, there are potential side effects that can occur following laser eye surgery. These may include dry eyes, glare, halos around lights, and fluctuating vision. While many of these side effects diminish over time, some individuals may experience more persistent issues.
It is crucial for candidates to have realistic expectations and understand the potential for complications. Discussing these concerns with a qualified ophthalmologist can provide much-needed clarity and insight into what the surgery may entail. To know more about side effects click here.
Post-Surgery Care and Recovery
Post-surgery care is another critical component for ensuring positive results after laser eye surgery. Patients typically receive detailed instructions on eye care, including the use of antibiotic drops to prevent infection and anti-inflammatory medications to ease discomfort.
Most patients can resume normal activities within a few days; however, avoiding strenuous activities, swimming, and exposure to irritants for a set period is generally advised. Regular follow-up appointments are also essential to monitor the healing process and address any concerns that may arise.
Preparing for Laser Eye Surgery
Preparation for laser eye surgery involves several steps crucial to achieving the best outcome. Candidates should understand the importance of preparation and work closely with their healthcare teams to ensure a successful procedure.

Consultation and Evaluation
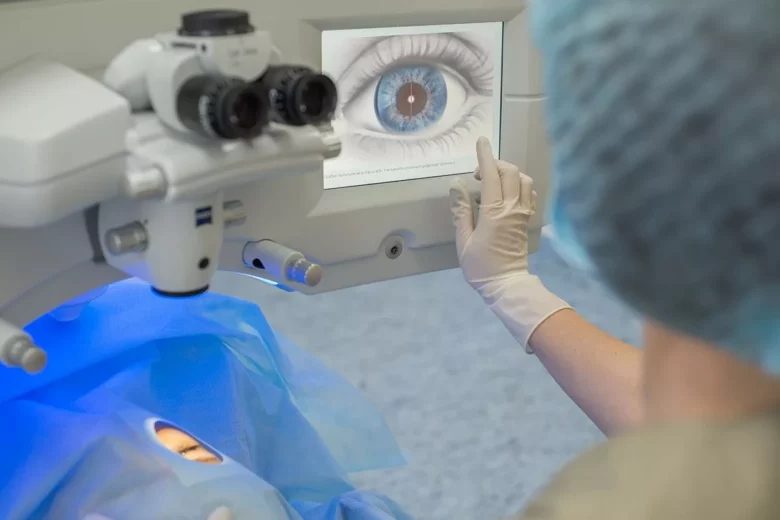
The initial step in preparation is undergoing a comprehensive eye examination. This evaluation typically includes various tests to assess the shape and thickness of the cornea, the overall health of the eyes, and the suitability for different types of laser procedures.
During the consultation, candidates should openly discuss their vision goals, medical history, and any concerns they might have regarding the surgery. This open line of communication will help the surgeon tailor recommendations and provide valuable information about what to expect.
What to Expect on Surgery Day
On the day of surgery, candidates will go through a series of pre-operative protocols that may include additional measurements and a brief discussion with the healthcare team. Patients are usually advised to have someone accompany them to help with transportation and aftercare.
Surgery typically takes less than an hour, and advanced laser technology means that the actual laser application only lasts a few seconds per eye. Following the surgery, patients will have an opportunity to rest before heading home with post-operative care instructions.