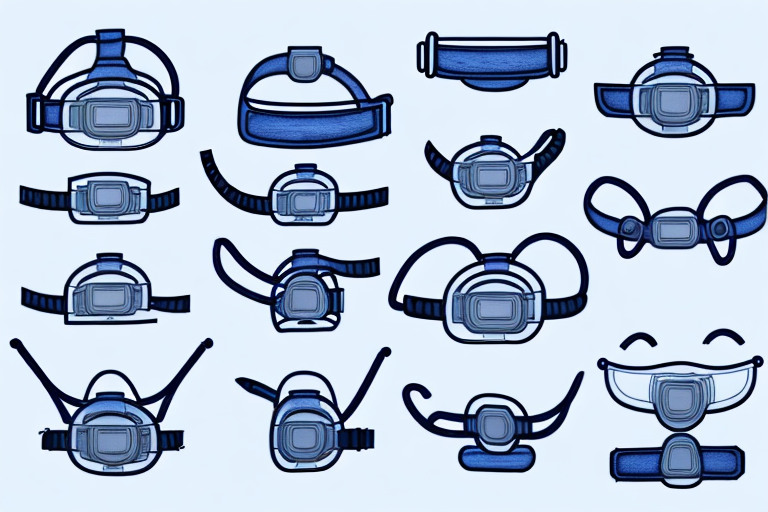
In the world of sleep apnea therapy, CPAP masks play a crucial role in ensuring restful and effective treatment. There are various types of CPAP mask online available, each with its own set of advantages and disadvantages. Understanding the differences and finding the right mask for your needs is an important step towards achieving optimal therapy.
Understanding CPAP Therapy
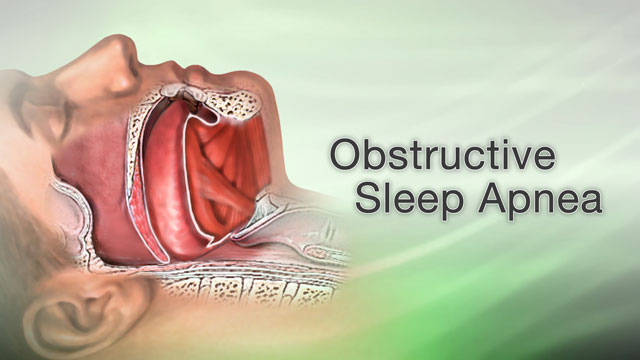
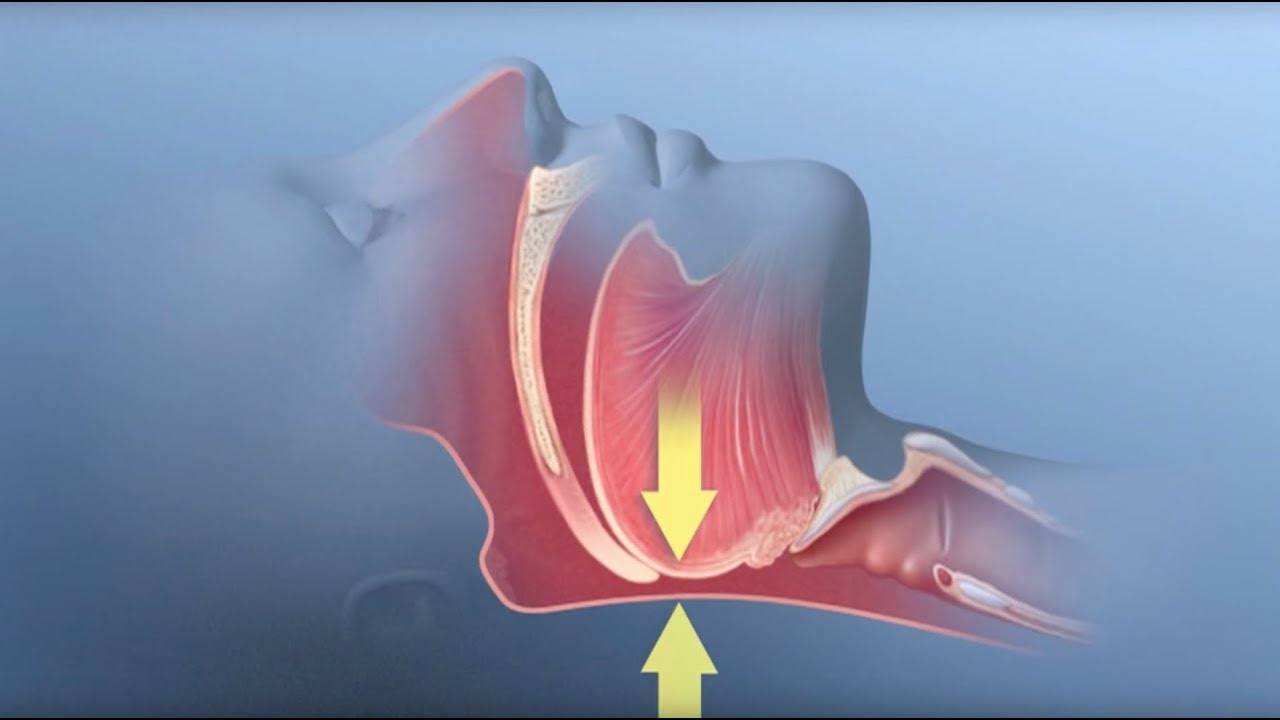
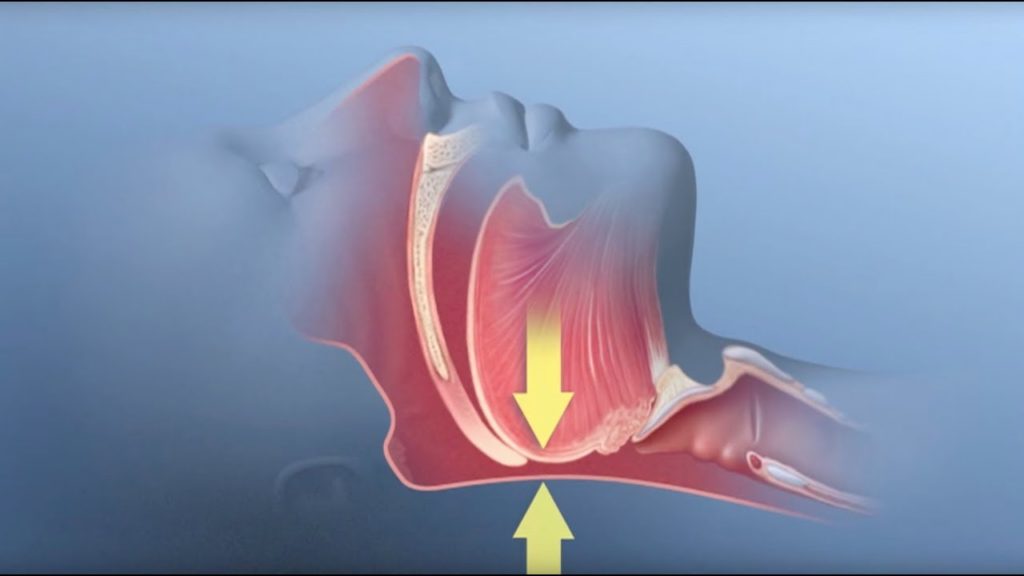
CPAP therapy, short for Continuous Positive Airway Pressure therapy, is the most common and effective non-invasive treatment for obstructive sleep apnea (OSA). It involves the use of a CPAP machine, which delivers a constant flow of pressurized air to keep the airway open during sleep. This continuous airflow prevents the collapse of the throat and helps individuals breathe more easily throughout the night.
What is CPAP Therapy?
CPAP therapy is a scientifically-proven method for managing OSA, a sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions, known as apneas, can lead to fragmented sleep, excessive daytime sleepiness, and other health complications.
During CPAP therapy, the CPAP machine generates a gentle stream of air that is delivered through a mask worn over the nose, mouth, or both. The pressurized air acts as a splint, keeping the airway open and allowing for uninterrupted breathing. This therapy is highly effective in reducing apneas and improving sleep quality.
It is important to note that CPAP therapy is not a cure for sleep apnea, but rather a way to manage its symptoms. Consistent and proper use of CPAP therapy can significantly improve the quality of life for individuals with OSA.
Importance of CPAP Masks in Therapy
CPAP masks act as the bridge between the CPAP machine and the user’s airway. They are responsible for delivering the pressurized air from the machine to keep the airway open. The choice of mask is critical to ensure comfort, proper fit, and compliance with therapy. Let’s delve into the different types of CPAP masks and explore their pros and cons. Click here to read more about CPAP Mask Cleaning and Maintenance: Best Practices for Prolonged Use.
Nasal masks are one of the most popular types of CPAP masks. They cover the nose and are secured with straps that go around the head. These masks are ideal for individuals who breathe through their nose during sleep. They provide a comfortable fit and allow for a wide field of vision. However, they may not be suitable for individuals who breathe through their mouth or experience nasal congestion.
Full face masks, as the name suggests, cover both the nose and mouth. They are recommended for individuals who breathe through their mouth or have difficulty breathing through their nose. Full face masks provide a secure seal and are less likely to be dislodged during sleep. However, some users may find them bulkier and less comfortable compared to nasal masks.
Nasal pillow masks are a newer option that deliver the pressurized air through small, soft nasal inserts that fit directly into the nostrils. These masks are lightweight, compact, and less intrusive compared to other types of masks. They are suitable for individuals who prefer minimal facial contact and have a tendency to feel claustrophobic. However, they may not be suitable for individuals with higher pressure requirements or those who experience nasal discomfort. You can also read about Sleep Apnea Machines: How They Can Improve Your Sleep Quality by visiting https://healthonlinezine.info/sleep-apnea-machines-how-they-can-improve-your-sleep-quality/
Oral masks, also known as hybrid masks, combine the features of nasal and full-face masks. They cover the mouth and have nasal prongs that fit into the nostrils. These masks are suitable for individuals who breathe through their mouth but also want the option of breathing through their nose. They provide a secure seal and allow for a more natural breathing experience. However, they may require adjustments to find the right fit and can be more expensive compared to other types of masks.
Choosing the right CPAP mask is crucial for a successful and comfortable therapy experience. It is recommended to consult with a healthcare professional or a CPAP equipment provider to determine the most suitable mask based on individual needs and preferences.
Overview of Different Types of CPAP Masks
When it comes to CPAP masks, there are three main types: nasal masks, full face masks, and nasal pillow masks. Each type has its own unique features and benefits that cater to different needs and preferences. Let’s take a closer look at each type to help you make an informed decision when selecting the right mask for your CPAP therapy.
Nasal Masks
Nasal masks are a popular choice for many CPAP users, thanks to their versatility and compact design. As the name suggests, these masks cover only the nose and are secured with straps over the head. They offer a comfortable fit and allow for easy movement during sleep. The open design of nasal masks also makes them suitable for individuals who wear glasses or enjoy reading or watching TV before bed.
One of the advantages of nasal masks is that they provide a more natural airflow, mimicking the way we naturally breathe through our noses. This can help reduce the feeling of air pressure and make the therapy more comfortable. However, it’s important to note that nasal masks may not be suitable for individuals with chronic nasal congestion or those who breathe through their mouth during sleep. In such cases, other mask options may be more appropriate.
Full Face Masks
Full face masks, as the name implies, cover both the nose and mouth, providing a broader coverage area. They are particularly ideal for individuals who breathe through their mouth while sleeping or those who experience frequent blockages in the nasal passages. With a full face mask, you can ensure that the pressurized air is delivered effectively, regardless of how you breathe.
One of the key benefits of full face masks is their ability to accommodate various sleep positions. Whether you sleep on your back, side, or stomach, these masks can provide a secure seal and maintain consistent therapy throughout the night. However, it’s worth mentioning that full face masks may feel bulkier compared to nasal masks, and some users may require an adjustment period to get used to the sensation of wearing them.
Nasal Pillow Masks
If you prefer a more minimalist approach, nasal pillow masks might be the perfect choice for you. These masks are the smallest and most lightweight option among CPAP masks. Instead of covering the entire nose or face, nasal pillow masks feature small cushion inserts that seal around the nostrils, delivering the pressurized air directly.
Nasal pillow masks are known for their minimal contact points, making them an excellent option for people who dislike the feeling of a mask on their face. They also tend to be quieter compared to other mask types, which can be beneficial for light sleepers or those who share a bed with a partner. However, it’s important to consider that nasal pillow masks may not be suitable for individuals with higher pressure needs or those who experience nasal discomfort. In such cases, alternative masks may be more appropriate.
When choosing a CPAP mask, it’s crucial to consider your individual needs, preferences, and comfort. Consulting with a healthcare professional or a CPAP equipment provider can also provide valuable guidance in selecting the right mask for your specific requirements. Remember, finding the perfect mask is an essential step towards successful CPAP therapy and a good night’s sleep.
Must Read:
Health Benefits of Oranges Nutritional Value of Orange
Deep Dive into Nasal CPAP Masks
Now let’s explore nasal CPAP masks in more detail to understand how they work and their pros and cons.
When it comes to treating sleep apnea, nasal CPAP masks are a popular choice. These masks are specifically designed to deliver pressurized air directly through the nostrils, ensuring an efficient airflow that helps keep the airway open during sleep. By creating a seal around the nose, these masks effectively deliver the required air pressure to prevent the collapse of the upper airway, allowing for uninterrupted breathing throughout the night.
The design of nasal CPAP masks is focused on comfort and usability. The mask’s cushion rests gently against the nose, providing a soft and comfortable fit. Additionally, adjustable headgear is used to keep the mask securely in place, allowing users to move around during sleep without worrying about the mask shifting or becoming dislodged.
One of the main advantages of nasal CPAP masks is their lightweight and compact design. Compared to other types of masks, such as full face masks, nasal masks are less obtrusive and easier to travel with. Their smaller size also means less material covering the face, providing a more open and less claustrophobic experience for users.
Furthermore, nasal CPAP masks are an excellent choice for individuals who tend to breathe through their mouth while sleeping. These masks are designed to specifically target the nasal passages, ensuring that the pressurized air is delivered directly to where it is needed most. By keeping the mouth free, nasal masks can help reduce dry mouth and increase overall comfort during therapy.
However, it is important to consider certain factors before choosing a nasal CPAP mask. Individuals with nasal congestion or allergies may find it challenging to use these masks effectively. Nasal congestion can obstruct the nasal passages, making it difficult for the pressurized air to reach the airway properly. In such cases, it may be necessary to use nasal decongestants or consider alternative mask options that allow for mouth breathing.
In conclusion, nasal CPAP masks offer a comfortable and effective solution for individuals with sleep apnea. Their lightweight and compact design make them a popular choice for those who value convenience and ease of use. However, it is crucial to consider individual needs and preferences, as well as any existing nasal conditions, to ensure that the chosen mask is the most suitable option for effective therapy. You can also read about Chronic obstructive pulmonary disease (COPD) by clicking here.
Exploring Full-Face CPAP Masks
Now let’s dive into the world of full-face CPAP masks and explore their functionality and advantages and disadvantages.

Functionality of Full Face CPAP Masks
Full face CPAP masks cover both the nose and mouth, ensuring a steady supply of pressurized air for individuals who breathe through their mouth or experience nasal congestion. These masks utilize a cushion that seals around the face, distributing the airflow evenly. Full face masks are designed to provide a secure seal, even when changing sleep positions during the night.
Advantages and Disadvantages of Full Face CPAP Masks
Full face CPAP masks offer a practical solution for mouth breathers and individuals who struggle with consistent nasal breathing. They provide a wider coverage area, reducing the likelihood of air leaks and ensuring effective therapy even when changing sleep positions. However, full face masks may feel bulkier and may require more adjustment to find the right fit. They can also be more prone to air leaks if the seal is not properly maintained.
Understanding Nasal Pillow CPAP Masks
Lastly, let’s explore the features, benefits, and drawbacks of nasal pillow CPAP masks.
The Design and Use of Nasal Pillow CPAP Masks
Nasal pillow CPAP masks consist of small, lightweight inserts that seal around the nostrils, delivering the pressurized air directly. These masks are designed to minimize contact points on the face, offering a barely-there feel during sleep. Nasal pillow masks often come with adjustable headgear to ensure a secure fit.
Benefits and Drawbacks of Nasal Pillow CPAP Masks
Nasal pillow CPAP masks are a popular choice for individuals who prefer minimal contact and unrestricted field of vision during sleep. They are lightweight, compact, and tend to be more comfortable for those who sleep on their side. However, nasal pillow masks may not be suitable for those who require higher levels of air pressure or for individuals who experience nasal discomfort or irritation.In conclusion, finding the right CPAP mask is crucial for effective and comfortable therapy. Nasal masks, full face masks, and nasal pillow masks each offer their own set of advantages and disadvantages. You can also read about Assessment of the Performance of Nasal Pillows at High CPAP Pressures by visiting https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746714/
Considering factors such as individual breathing patterns, comfort preferences, and the severity of nasal congestion will help you make an informed decision. Remember, consulting with a healthcare professional or CPAP specialist can provide valuable guidance in selecting the most suitable mask for your specific needs.