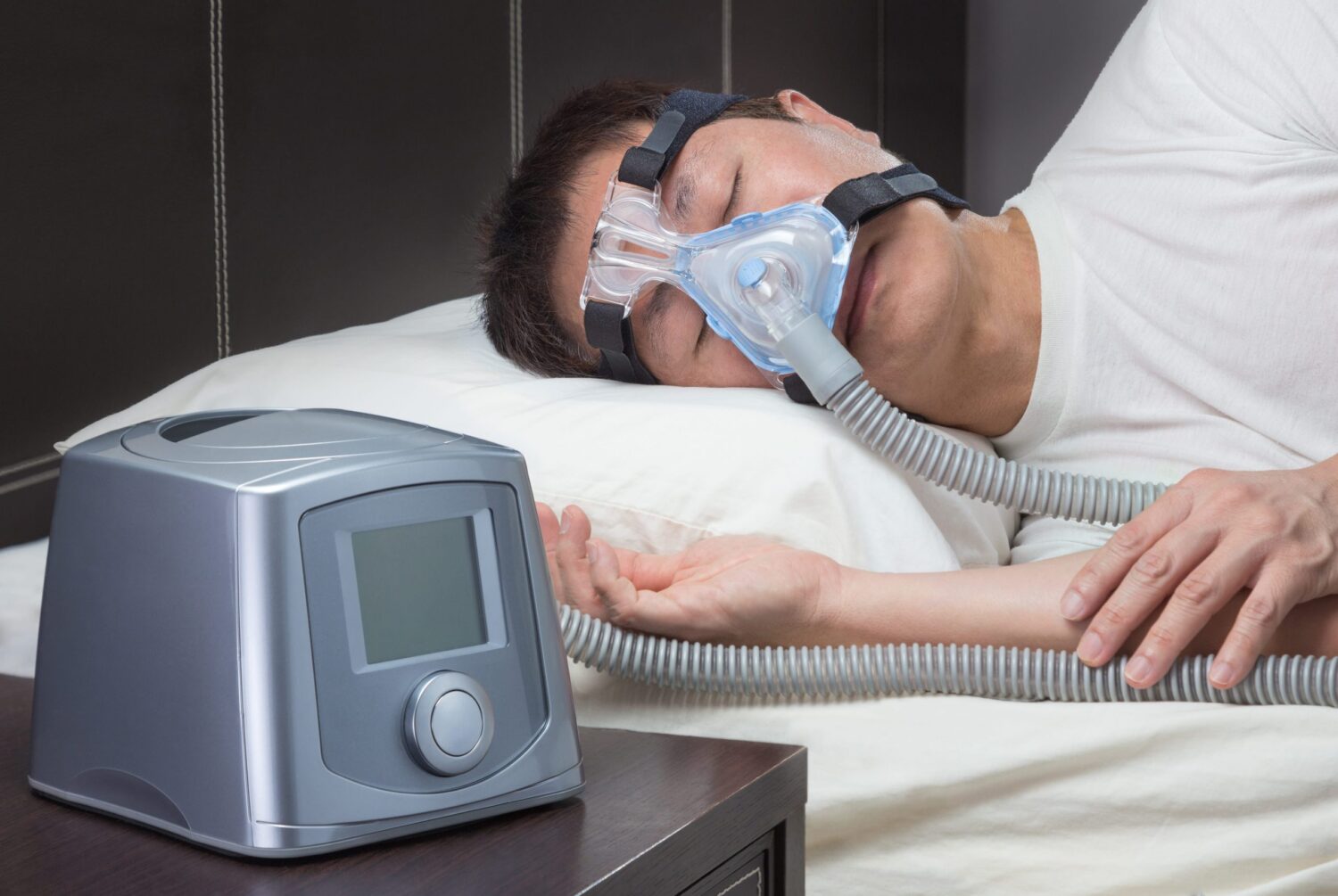
If you or a loved one suffer from sleep apnea, you know just how important reliable and efficient CPAP therapy is. But what if you need to travel, or you simply want to enjoy the convenience of a smaller, more portable CPAP device? That’s where the ResMed AirMini comes in.
Introduction to the ResMed AirMini
The resmed airmini is a revolutionary device that has changed the game for those who suffer from sleep apnea. It is a top-of-the-line portable CPAP device that offers many of the same features and benefits as its larger counterparts, but in a small and lightweight design that is perfect for travel or everyday use. The AirMini is designed to provide effective therapy for sleep apnea in a compact and convenient package, making it an ideal choice for those who are always on the go.
What is the ResMed AirMini?
The ResMed AirMini is a portable CPAP device that delivers highly effective therapy for sleep apnea in a small, lightweight package. Using advanced technology and innovative design, the AirMini is able to deliver the same level of therapy as larger devices, but in a travel-friendly form that can easily fit in your carry-on bag. The AirMini is designed to be user-friendly and easy to use, making it an ideal choice for anyone who needs to use a CPAP device on a regular basis.
The AirMini is equipped with a range of advanced features that make it one of the most effective and reliable CPAP devices on the market. These features include AutoRamp, which helps you fall asleep more comfortably by gradually increasing the pressure of the air as you fall asleep, and SmartStart, which allows you to start and stop therapy simply by breathing into the mask. Click here to read more about Sydney eye clinic: Top eye clinics you need to know.

Why Choose a Portable CPAP Device?
While traditional CPAP machines are effective at treating sleep apnea, they can be bulky and difficult to transport. Portable CPAP devices like the ResMed AirMini offer a convenient and travel-friendly solution that allows you to maintain your treatment even when you’re on the go. Whether you’re traveling for work or pleasure, or you simply want a smaller option for everyday use, the ResMed AirMini provides all the power and features you need to experience the benefits of CPAP therapy.
The AirMini is also incredibly quiet, making it easy to use without disturbing your partner or anyone else in the room. It is also incredibly easy to clean and maintain, with a simple and intuitive design that makes it easy to disassemble and reassemble for cleaning.
Overall, the ResMed AirMini is an excellent choice for anyone who needs a portable and reliable CPAP device. With its advanced features and user-friendly design, it is sure to provide you with the effective therapy you need to get a good night’s sleep, no matter where you are.
Key Features of the ResMed AirMini
Compact Size and Lightweight Design
The ResMed AirMini is not only one of the smallest CPAP devices on the market, but it is also incredibly lightweight, weighing in at just 0.66 pounds. This makes it the perfect choice for those who are always on the go or who love to travel. You can easily pack it in your luggage or carry-on without worrying about taking up too much space or adding extra weight to your bag. Additionally, its compact design makes it perfect for use at home, as it won’t take up much space on your bedside table or nightstand.
Despite its small size, the ResMed AirMini still delivers powerful therapy to help you get the best sleep possible. Its compact size and lightweight design make it an ideal choice for those who want to maintain their active lifestyle without sacrificing quality sleep.
SmartStart and AutoRamp Technology
The ResMed AirMini features SmartStart technology, which allows therapy to begin once you start breathing into your mask. This eliminates the need to press any buttons or adjust settings manually, making it easy to use and convenient for those who need to start therapy quickly. Additionally, the AirMini includes AutoRamp technology, which gradually increases pressure as you fall asleep, ensuring a comfortable and effective experience.
With SmartStart and AutoRamp technology, you can rest easy knowing that your therapy will begin seamlessly and that the pressure will adjust to your needs throughout the night. This feature is especially beneficial for those who have trouble falling asleep or who need a little extra help adjusting to therapy.
HumidX Waterless Humidification System
The ResMed AirMini is designed to provide optimal comfort and therapy without the need for a bulky water chamber. Instead, it uses the HumidX waterless humidification system, which delivers moisture to your airways without adding extra weight or hassle to your device. This makes it incredibly convenient for travel, as there is no need to worry about filling the water chamber or finding distilled water on the go.
The HumidX waterless humidification system is also incredibly easy to use. Simply insert the HumidX cartridge into your mask and you’re ready to go. The cartridge will last for up to 30 days, making it a cost-effective and hassle-free option for those who want to enjoy the benefits of humidification without the extra maintenance.

Expiratory Pressure Relief (EPR)
The ResMed AirMini includes Expiratory Pressure Relief (EPR), which reduces your pressure while exhaling, resulting in a more natural and comfortable breathing experience. This feature is especially beneficial for those who have trouble adjusting to CPAP therapy, or who experience discomfort from high pressure levels.
EPR works by lowering the pressure delivered by the device as you exhale, making it easier for you to breathe out. This can help reduce discomfort and make therapy more comfortable overall. With EPR, you can enjoy the benefits of CPAP therapy without worrying about discomfort or pressure-related issues.
Built-in Bluetooth Connectivity
The ResMed AirMini includes built-in Bluetooth connectivity, allowing you to track your sleep data and adjust your settings using the AirMini app. This makes it easy to customize your therapy and get the most out of your device, whether you’re at home or on the go.
The AirMini app is incredibly user-friendly and allows you to monitor your sleep data, adjust your settings, and even troubleshoot any issues you may be experiencing. With built-in Bluetooth connectivity, you can stay connected to your therapy and ensure that you’re getting the best sleep possible.
Customizing Your ResMed AirMini Experience
The ResMed AirMini is a revolutionary CPAP machine that provides effective therapy in a compact and portable design. While it’s important to use your AirMini consistently to achieve the best results, there are many ways to customize your experience to make it even more effective and comfortable. Here are some tips for getting the most out of your ResMed AirMini:
Choosing the Right Mask and Accessories
One of the most important aspects of using the ResMed AirMini is finding the right mask and accessories to suit your individual needs. There are many options available, including nasal masks, full face masks, and pillows masks, each with their own unique benefits and drawbacks. It’s important to work with your healthcare provider to find the best fit for your individual needs. They can help you determine which mask style is most suitable for your sleeping habits and facial structure, and recommend any necessary accessories to enhance your therapy experience.
For example, if you tend to breathe through your mouth at night, a full face mask may be a better option for you. Alternatively, if you prefer a more minimal design, a nasal mask or pillows mask may be a better fit. Additionally, there are many accessories available for the AirMini, including travel bags, battery packs, and external power supplies, which can enhance your experience and make it even more convenient.
Adjusting Pressure Settings and Modes
The ResMed AirMini allows you to adjust your pressure settings and modes to customize your therapy based on your individual needs. This is important because everyone’s breathing patterns and sleep habits are unique, and may require different pressure levels to achieve optimal therapy.
Whether you need to increase pressure levels to combat obstructive apneas, or reduce pressure to make your therapy more comfortable, the AirMini offers a wide range of settings and modes to help you achieve the best results possible. Your healthcare provider can help you determine which settings are most appropriate for your individual needs, and provide guidance on how to adjust them as necessary.
Using the AirMini App for Personalization and Tracking
The AirMini app is a valuable tool that allows you to track your sleep data, adjust your therapy settings, and get helpful insights into your sleep habits. With the app, you can view your therapy progress, monitor your mask seal, and even receive tips for improving your sleep hygiene.
Whether you’re at home or on the go, the AirMini app can help you get the most out of your device. You can use it to adjust your pressure settings, track your sleep data over time, and even connect with your healthcare provider for remote monitoring and support. With the AirMini app, you can take control of your therapy and achieve better sleep health.

Maintaining and Cleaning Your ResMed AirMini
Daily and Weekly Cleaning Recommendations
To ensure optimal performance and hygiene, it’s important to regularly clean and maintain your ResMed AirMini. This includes daily cleaning of your mask and tubing, as well as weekly cleaning of your device’s air filter and humidification system. It’s also important to inspect your device regularly to ensure that all components are functioning properly and that there are no leaks or other issues.
Replacing Filters and Accessories
Over time, your ResMed AirMini will require replacement filters and accessories to keep functioning effectively. It’s important to follow the manufacturer’s recommendations for replacement intervals, and to purchase only genuine ResMed filters and accessories to ensure compatibility and reliability.
Troubleshooting Common Issues
If you experience any issues with your ResMed AirMini, there are many resources available to help you troubleshoot and resolve the problem. From the user manual to customer support, there are many ways to get the help and guidance you need to get the most out of your device.
In Conclusion
The ResMed AirMini is an excellent choice for those who require reliable and efficient CPAP therapy, but want the convenience and portability of a smaller device. With its advanced features and innovative design, the AirMini offers all the power and effectiveness of larger machines in a compact and travel-friendly package. By following the tips and advice in this guide, you can get the most out of your ResMed AirMini and enjoy the many benefits of CPAP therapy wherever life takes you.